A 60yr(M) chronic Alcoholic with Abdominal Distension
THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT
Complaints-
A 60yr old male came with complaints of -abdominal distension
-decreased urine output since 4 months
-Swelling of B/L lower limbs
HOPI -
Patient was aparently asymptomatic 4 months back.He then developed abdominal distension which was insiduous in onset , gradually progressive associated with pain abdomen- squeezing type in umbilical region , aggravted on taking food with no releiving factors .
H//O decreased urine output since 4 months
H/O EDEMA in B/L lower limbs - Pitting type extending upto knee level with no aggravating pr releving factors.
H/O SOB on exertion - Grade 3 MMRC
H/O Fever since 10 days - low grade , intermittent associated with chills and rigors and releived by medication .
H/O Burning micturition since 1 month
H/O cough with expectoration since 4 to 5 days whitish sputum, non blood tinged.
No H/O Nausea, vomitings , Chest pain, palpitations, Giddiness , Sweating
Past History-
No similar complaints in the past
K/C/O Type 2 DM and HTN since 1year
Not om regular medication.
N/K/C/O - TB, Asthma, Epilepsy, CVA, CAD, Thyroid disorders.
Treatment History- H/O Blood Transfusion done 3 months back -uneventful
Personal History-
Diet- Mixed
Appetite- Decreased since 2months
Bowel & Bladder Movements-H/O Constipation since 1 month ( passing stools once in 3 days) &Decreased urine output since 4months and burning micturition since 1month
Sleep - Adequate
Addictions - Chronic Alcoholic Since past 40 years consumed around 90 to 120ml/day
H/O Smoking since past 35yrs
Family history- Not Significant
GENERAL EXAMINATION-
Patient is Conscious, Coherent and Co operative .
Pallor present
Pedal Edema - Present Pitting type
No signs of ,Icterus Clubbing, Cyanosis, Lymphadenopathy
Vitals-
TEMP: Afebrile
BP: 140/70mmHg
PR: 102 bpm
RR- 24cpm
Spo2- 96% @RA
GRBS:485mg/dL
Systemic Examination:
CVS: Inspection
Chest wall is bilaterally symmetrical.
No precordial bulge is seen
Palpation
JVP- Normal
Apex beat -felt in the left 5th intercoastal space in the mid clavicular line
Auscaltation-
S1&S2 are heard,no murmur found.
RESPIRATORY SYSTEM
Position of trachea- central
Bilateral air entry, normal vesicular breath sounds are heard.
No added sounds
CNS
Patient is conscious ,coherent and co operative , well oriented to time and space.
Speech normal.
No signs of meningeal irritation.
Motor and sensory system- Normal
Reflexes - present
Cranial nerves - intact
PER ABDOMEN
On inspection:
Abdominal distention - Present
Abdominl Girth 85cms
All quadrants are moving equally with respiration
Umbilicus - central and inverted
Engorged Veins present
No scars, prominent Venous pulsations and visible peristalsis.
On palpation::
Superficial palpation- No Local rise in temperature and no tenderness
Deep palpation- No guarding, rigidity
On percussion::
Tympanic note - heard
Shifting Dullness present
On auscaltation::
Bowel sounds heard
Provisional Diagnosis-
Chronic liver disease with Portal Hypertension and Anemia.
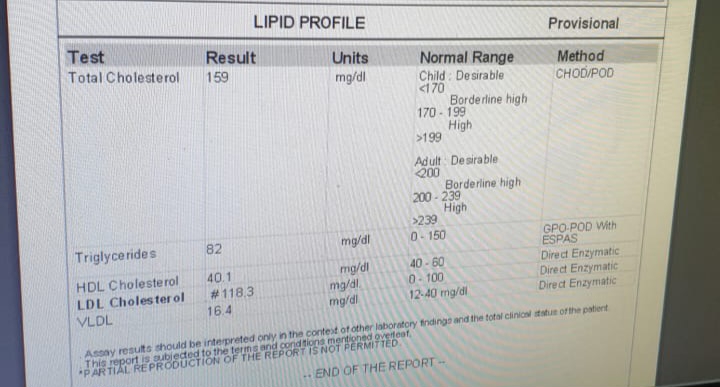
Investigations
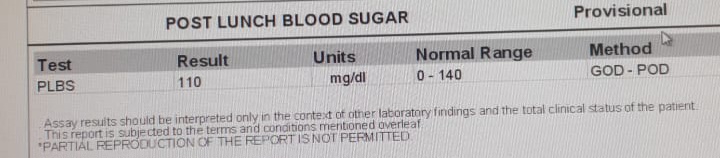
RBS
Hemogram -7/07/2023
280ml of PRBC transfusion done (Uneventful)
Hemogram - 9/07/2023
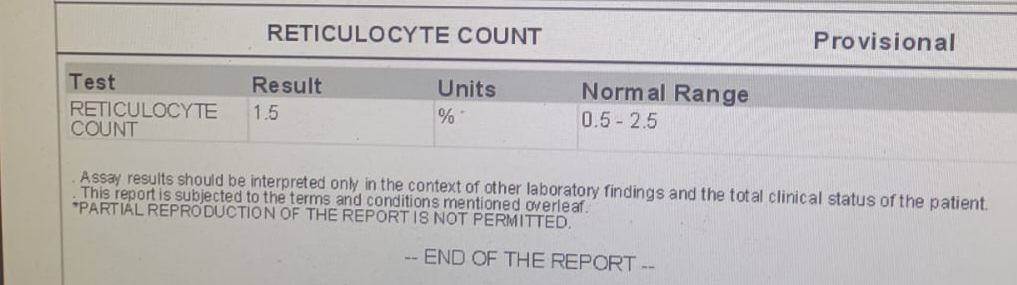
Blood GroupingReticulocyte count
APTT -07/07/2023
Ascitic Tap done on 8/07/2023 -1L of ascitic fluid collected.
Ascitic Fluid for LDH
Treatment-
1.Inj- HAI 6units IV/STAT
2.Inj.HAI SC/TID
3.Tab.LASIX 40mg PO/BD
4.Tab.PCM 650mg PO/OD
5. GRBS monitoring .











 8/07/2023
8/07/2023




















Comments
Post a Comment